Curious to explore the undersea world, Alexander the Great used a glass diving bell to submerge himself below the surface. The fish, it is said, “crowded around him in homage.” In 332 BCE, he ordered soldiers to submerge inside diving bells and destroy the enemy’s underwater defenses.
DEPTH Blog
Raja Ampat is a special place. Author Jennifer Idol is traveling this week to share her experiences exploring the cradle of our oceans.
"Current philosophy dictates that all dives, even those well within the no-stop limits of tables and computers, should include a controlled ascent (dictated by the diver's computer, tables, or personal or training philosophy) and a safety stop. Newly published research recommends slower ascent rates (slower than 60 feet, or 18.2 meters, per minute according to most tables) possibly coupled with multiple safety stops. Reading available data published by the training associations and DAN is a good way to become familiar with the latest information on ascent protocols.
Author Paul Mila, wrote Harry Hawksbill Helps His Friends to impart both a social message for young children and also to teach them about sea life.
Scientific divers often work in remote areas, and sometimes far offshore.
Author Jennifer Idol has taken the dive industry by storm since last year (2016) when she published her first book, An American Immersion. Today, Jennifer shares a few insights on how to get your first book published (and a few photos from her dive near the Best Publishing Company HQ). . .
Content is being consumed in more dynamic ways than ever before and new methods must be used to engage readers.
"The ability to manage a diving emergency and provide care to an injured diver does not come from experience alone. The best thing you can do to prepare for the dive-related injuries is to learn everything you can about such injuries and the situations that lead to them.
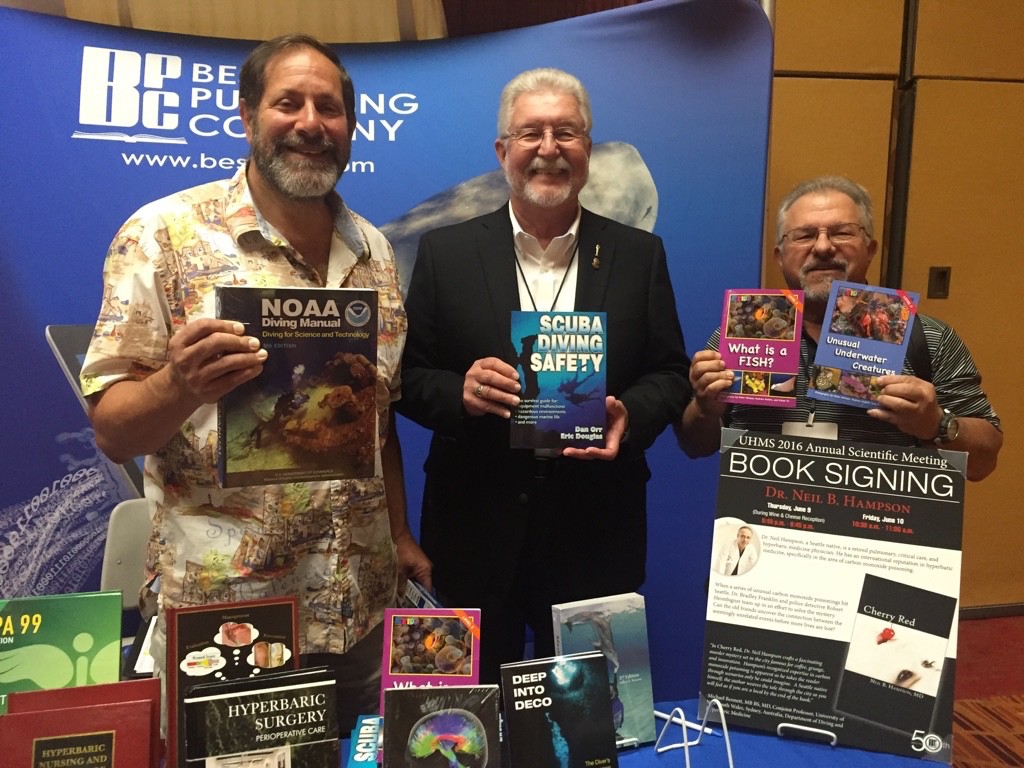
John Heine, author of Cold Water Diving: A Guide to Ice Diving, travels to places such as Antarctica (pictured below) to oversee scientific diving through the U.S. Antarctic Program of the National Science Foundation. In the photo belog he is researching the use of rebreathers under the ice, as well as various new strategies to stay warm with the use of active (electric) heated undergarments.
More than 100 years ago, Sorbonne Professor Paul Bert, the father of pressure physiology, explained, “All symptoms, from the slightest to those that bring on sudden death, are the consequences of the liberation of bubbles of nitrogen in the blood [on-gassing], and even in the tissues, when compression has lasted long enough. The great protection is slowness of decompression [off-gassing].”
When author Paul Mila was writing Harry Hawksbill Helps His Friends, he and the Best Publishing Company editorial staff wrestled with one main question: should we use his underwater photographs to tell the story, or retain the services of an illustrator?
Jennifer Idol shares two questions that she is most frequently asked about her 50 state journey:
In the below image a scientific diver works in a deep kelp bed in central California. She is measuring the percent cover of various marine algae as a part of her Master’s thesis.
In 1982, when David Scalia was evacuated to San Diego after suffering an air embolism to his brain, there was no hyperbaric chamber in the city.
"The signs of emergencies are varied and can be subtle. They may be apparent before or during the dive. A diver's ego or peer pressure may cause the diver to disguise a problem, such as a lack of competence, inadequate experience, overconfidence, anxiety, illness, or distress. Such problems may show up on the boat before anyone gets in the water. All divers should adopt the credo of the cave and technical diving communities: Any diver can call any dive for any reason at any time. No question are asked - and the credo applies before the dive even begins. All divers should agree to this as part of the predive briefing. If more divers felt comfortable not making a dive because it was beyond their experience, or they didn't feel well, or their karma was all wrong, or whatever, there would probably be fewer problems."
A textbook may sometimes gain the unusual trait of longevity beyond all other books — it can be revised
and remain a primary source of information for generations of students.
What does it look like to write a book?
If you're a diver, you've most likely heard of the "bends" or "divers disease."
Get an exclusive sneak peek of this newly created 7-minute film by Jennifer Idol about her journey diving across all 50 states. Jennifer has not shared this video with many people outisde of her personal circle.